William French, MD - Anticoagulation: Special Populations - Figure 25
Triple Antithrombotic Therapy
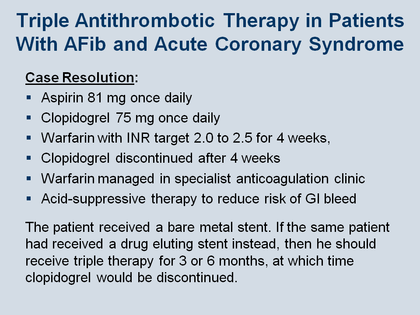
This Figure shows the clinical resolution of the patient case presented in Figure 20. The first choice the clinicians managing this patient made was to use low-dose aspirin (81 mg once daily), because in general, the higher the aspirin dose, the greater the chance of having a GI bleed.
The second choice was to add another antiplatelet agent. With any of these – clopidogrel, prasugrel, or ticagrelor – it is necessary to stay with the so-called maintenance dose. In the case of clopidogrel this is 75 mg once a day, and there are no data suggesting that it is possible to lower that dose and still get prophylaxis against stent thrombosis. So physicians have to understand that they must maintain the standard antiplatelet regimen with the secondary antiplatelet agents such as clopidogrel, prasugrel, or ticagrelor, on top of the low-dose aspirin regimen.
The third choice then was warfarin, maintaining the INR target in the lower range of 2 to 2.5 (realizing the therapeutic range still remains 2 to 3), and to do this for 4 weeks. The challenge with trying to maintain a patient’s INR target between 2 and 2.5 is that this is easily said but difficult to achieve – it is hard simply to keep many patients within the target range of 2 to 3. The important challenge when targeting the lower range of 2 to 2.5 is the tendency to undershoot the target, with the result that the patient is in a subtherapeutic INR and at higher risk of having thromboembolic event.
The fourth clinical decision point was to discontinue clopidogrel after 4 weeks. The reason for this was that the patient was treated with bare-metal stents. Bare-metal stents generally endothelialize within 4 weeks, so the concept of stopping clopidogrel was based on earlier recommendations, although the current guidelines suggest even though endothelialization may be more complete earlier in patients with bare-metal stents than with drug-eluting stents, the guidelines still recommend 12 months of clopidogrel. So, recalling that this patient has 2 out of 5 bleeding risks (Figure 23), he will be at higher risk of having a bleed on triple therapy, and this was the reason for stopping clopidogrel at 4 weeks.
Finally, this patient’s warfarin was managed in a specialist anticoagulation clinic. It has been shown that the specialist anticoagulation clinics do a better job overall in managing patients and generally have a higher rate of keeping patients within the so-called “time in therapeutic range” (TTR).
In addition, and probably a little more controversially, this patient was given acid-suppressive therapy to reduce risk of GI bleeding. There are data suggesting that, in patients who are on a clopidogrel-like agent, reducing acid secretion in the stomach with appropriate therapy leads to less GI bleeding.
If this patient had received a drug-eluting stent instead of a bare-metal stent, the triple therapy would have to be continued for 3 or 6 months, depending on the make of the stent, and not continued for the entire year. Again this is somewhat controversial and not exactly what the guidelines suggest at this time.
French WJ. Am J Med 2013; 126: 00-00.