William French, MD - Anticoagulation: Special Populations - Figure 20
Anticoagulation and ACS/CAD
ACUTE CORONARY SYNDROME (ACS) and CORONARY ARTERY DISEASE (CAD)
The final subset of patients with AFib that present special challenges to physicians and the healthcare system are those patients with ACS or CAD who may need to be treated with both antiplatelet therapy (for ACS and/or CAD) and with antithrombin therapy (for AFib, for example). Because this typically involves 2 kinds of antiplatelet therapy (either aspirin with clopidogrel, prasugrel, or ticagrelor as the two antiplatelet agents) plus an antithrombin/anticoagulant agent, it is referred to as “triple therapy.”
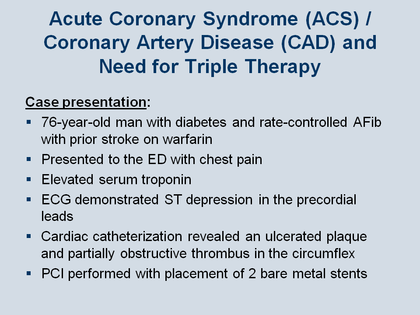
To illustrate this conundrum, the Figure outlines a recently published case presentation: a 76-year-old man who has diabetes and rate-controlled AFib with a prior stroke who was on warfarin.[133] In other words, the patient was being treated with warfarin because of his prior stroke and the finding of AFib. Then, on a different day, he presented to the emergency department with chest pain, where he was found to have an elevated serum troponin level and an ECG tracing demonstrating ST segment depression in the precordial leads. The patient went to the cardiac catheterization lab (which was appropriate) and that revealed an ulcerated plaque rupture with partially obstructed thrombus in the left circumflex coronary artery with a significant obstruction. The patient underwent immediate percutaneous coronary intervention (PCI) and placement of two bare-metal stents.
The clinical question: in sending this patient, who is already on an antithrombin therapy because of his AFib, to the cath lab for an invasive procedure (PCI) for his ACS, with implantation of a bare metal stent, which requires a period of antiplatelet therapy, what should be the strategy for this “triple therapy”?
French WJ. Am J Med 2013; 126: 00-00.